In summer 2024, an 8-year-old boy with a giant cerebral aneurysm was referred to Children’s Medical Center Dallas, part of Children’s Health℠, for neurosurgical evaluation.
Rafael Sillero, M.D., Pediatric Neurosurgeon at Children’s Health and Assistant Professor at UT Southwestern, cared for the child in the center’s new neurosurgery hybrid OR. The hybrid setup – the only one in Texas dedicated to pediatric neurosurgery – enabled Dr. Sillero to combine multiple techniques in a single operation and achieve an exceptional clip reconstruction.
The efficiency and precision demonstrated in this case would not have been possible in standard facilities where imaging, endovascular procedures and surgery take place at different times and places.
“Cases like these show that hybrid ORs elevate the standard of care for pediatric neurosurgery,” says Dr. Sillero. “More centers should commit to building this capability so that more children can avoid the risks inherent in the status quo.”
Why it matters: Hybrid ORs prevent delays and risks
Surgeries for aneurysms, arteriovenous malformations (AVM) and brain tumors rely on postoperative imaging to verify results. Typically, this means conducting the craniotomy, closing the surgery – and transferring the patient for imaging.
If angiography reveals residual lesions in need of resection or repair, the patient requires a second operation.
“In the meantime, the child is at risk of events like brain bleeds that cause life-threatening damage,” says Dr. Sillero.
Hybrid ORs reduce the risks and delays of standard neurosurgery by combining all the necessary resources in one room.
Patient example: Catastrophic rupture avoided thanks to Hybrid OR
The child with the giant cerebral aneurysm required surgery to avoid a catastrophic rupture. Dr. Sillero combined two techniques that are impossible to integrate outside a hybrid OR.
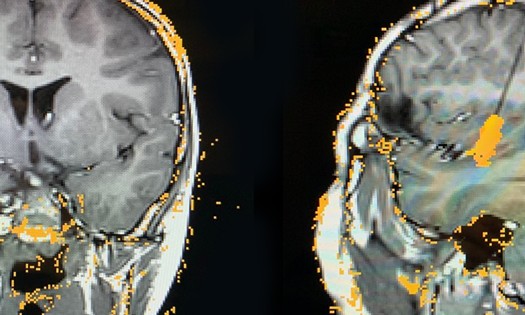
The child had a complex middle cerebral artery bifurcation with one branch arising from the dome of the aneurysm. Dr. Sillero had to determine whether it was safe to clip the artery to prevent blood flow to the aneurysm, or whether clipping would also limit blood flow to the rest of the brain. The typical method is to test endovascularly – but access can be difficult.
In the hybrid OR, Dr. Sillero:
Placed a temporary clip on the artery during an open craniotomy.
Performed an angiogram to observe neuromonitoring changes.
Confirmed that a bypass was unnecessary and that clipping could proceed without preserving the artery.
The perioperative angiogram meant Dr. Sillero didn’t have to close the surgery and wait to confirm there was no residual sac from the aneurysm.
“I simply rotated the patient table and got the images then and there,” he says.
Thanks to the hybrid approach, Dr. Sillero achieved an exemplary clip reconstruction. Months later, the patient is thriving with no evident risks.
Why Children’s Health: Pioneers in pediatric neurosurgery
Children’s Health opened its hybrid neurosurgery OR in spring 2024 and immediately shifted all vascular cases to this room.
“The benefits are so strong – you want the hybrid OR for every patient. It is definitely our standard of care at Children’s Health now,” explains Dr. Sillero.
The room features biplane X-ray capability for more comprehensive angiography. It is also bigger than the typical OR to accommodate additional neuromonitoring and neuronavigation equipment.
Altogether, the hybrid OR provides three game-changing benefits:
Greater efficiency and precision
Reduced risk of reoperation and emergent events
Access to all treatment modalities
Dr. Sillero says the third point helps neurosurgery transcend any unintentional bias of the physician who leads the patient’s care.
“In a traditional setting, it’s the old problem of when you have a hammer, everything looks like a nail: Interventional radiologists are biased toward their treatment modalities, while surgeons are biased toward the approaches they know best,” he explains.
In the hybrid OR, all the expertise and tools come together in one room. Dr. Sillero is dual trained in surgical and endovascular procedures – but other pediatric centers will have separate specialists scrubbing in and out or working in tandem (depending on the patient’s needs). For conditions like juvenile nasopharyngeal angiofibroma, Dr. Sillero collaborates with an otolaryngologist.
“You can work together and pivot to whatever care is best for the patient. That is the standard we should all follow in every case,” says Dr. Sillero.